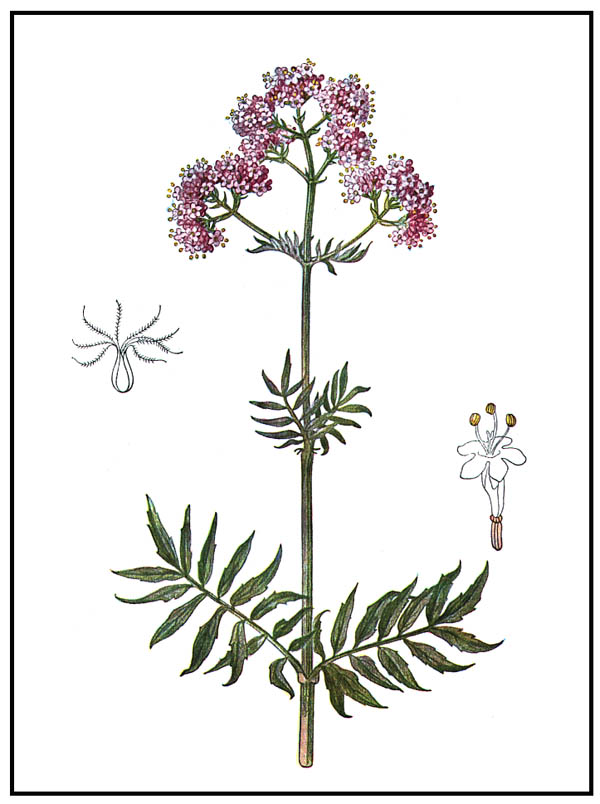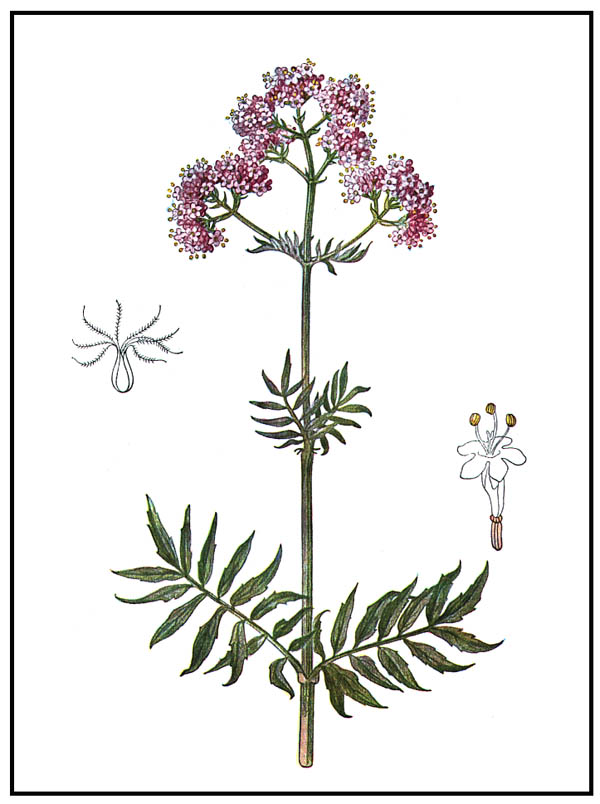
Figure 1: Valeriana officinalis.
VALERIAN AND NARDOSTACHYS
Almost everyone is familiar with the herb valerian, used for its calming and antispasmodic properties. It is taken in the form of tea, tincture, capsules, or tablets to treat nervousness and insomnia, muscle spasms, and pain. Valerian is one of the principal herbs of the Western tradition, rated among the top 10 herbs in America and Europe (along with garlic, ginkgo, St. John's wort, and echinacea). While valerian is used in the Far East to only a limited extent, an "Oriental valerian" is more commonly used there: it is a close relative called nardostachys. Nardostachys was known in ancient times as "nard" and, later, as spikenard (though other plants have also been given this name, so nardostachys is referred to as "true" spikenard).
Valerian and nardostachys belong to the Valerianaceae family, one which gives rise to relatively few herbal medicines, these two herbs being the main ones (a third herb, patrinia, is used in Chinese medicine). They share a group of active constituents and the herbs are each characterized by an unusual fragrance, derived from the essential oil component. Below is an overview of their constituents, pharmacology, and medicinal actions.
There are numerous species of Valerian that have been utilized by herbalists (of approximately 150 species found worldwide, about 20% have been recorded as used for medicinal purposes), but the most common one has been named the official species: Valeriana officinalis (see Figure 1). Other species of Valeriana may lack sufficient active constituents to make them as desirable. This herb is believed to be the one recorded by Dioscorides as phu, which refers to the peculiar strong odor of the root that combines pleasant and unpleasant fragrances. The herb may have been later named valerian after the Roman Emperor Valerian (Publius Licinius Valerianus; 253-260 A.D.), or both the herb and Emperor may have been named for their qualities (in Latin, valere means to be in health; valero means to be strong).
The herb was found to be valuable in the treatment of epilepsy in the Middle Ages, which may be considered the origin of its current use as an antispasmodic. In the modern era, valerian became known as a nervine, a term that implies that it could calm the nervous system while also acting as a tonic (something that strengthens the body; in this case, it would nourish and improve the function of the nervous system). A typical example of the application of nervines is for treatment of nervousness and insomnia that result from stress and overwork. The British herb specialist M. Grieve, in her 1931 publication, A Modern Herbal (1), relayed the use of valerian during the First World War: "When air-raids were a serious strain on the overwrought nerves of civilian men and women, valerian, prescribed with other simple ingredients, taken in a single dose, or repeated according to the need, proved wonderfully efficacious, preventing or minimizing serious results." The herb was used even more often during the next World War for the same purpose, and valerian has become the principal remedy for nervousness in European herbal medicine.
Although valerian is also known as an analgesic, more powerful pain-relieving medications have long been available (such as the morphine derivatives and the non-steroidal antiinflammatory drugs), so that it hasn't had much use for this purpose recently. While valerian's antispasmodic action was originally relied upon to treat convulsions and other serious disease symptoms, it is now applied to milder disorders, such as cases of gastro-intestinal spasms and minor peripheral muscular spasms. The majority of valerian research today is aimed at evaluating its potential to treat insomnia and anxiety (10). As a sleep aid, valerian is sometimes evaluated in combination with hops (Humulus lupulus) and/or lemon balm (Melissa officinalis) In the book Herbal Medicine (2), a number of double-blind, placebo-controlled studies of valerian's effect (alone or with hops; sometimes in larger formulas, containing lemon balm or other herbs) on sleep have been reviewed; a daily dose of about 400 mg of valerian extract (typically a 4:1 preparation) appears to be effective.
The major active constituents of valerian appear to fall into two broad groups:
The valepotriates are a type of iridoid (these are in the triester form; the iridoids in glycoside form are found in rehmannia, scrophularia, gardenia, and vitex, among other Chinese herbs used for clearing heat). These iridoids are thought to confer the primary sedative effect, though the essential oils, especially the sesquiterpenes, are also active. Typically, there is less than 1% of valepotriates and less than 1% of essential oils in the dried valerian roots. The mechanism of action of these compounds has not been fully elucidated, and the speculation about mechanisms will not be relayed here other than to indicate that changes in the levels of neurotransmitters appear to occur as a result of using the herb or its active components. Valerian is collected and cultivated world-wide as a medicinal plant, including Europe, Turkey, India, and China. It is manufactured into widely used medicinal formulations in Europe, particularly in Germany. A German text (9) points out that valerian tincture, a commonly used dosage form, needs to be taken in amounts of one to two teaspoons, rather than a few drops, to attain good results.
The famous aromatic root, nard, was known in ancient times as an ingredient in ointments, and is believed to be the same as the Indian nardostachys, N. jatamansi (see Figure 2) which has been renamed Nardostachys grandiflora. There is also a Valeriana jatamansi that is similar to nardostachys and used as a substitute. The species name jatamansi is adopted directly from the original Sanskrit name of the herb. The biblical nard was a costly aromatic ointment, preserved in alabaster boxes. Unlike valerian, which has an odor that is often described as unpleasant (sometimes likened to dirty socks), the nardostachys fragrance is considered attractive and similar to expensive musk. Its oil is used in perfumery (especially to fragrance women's hair); the herb is also used in bathwater and it is a major ingredient in incense. In India, it is used in making many massage oils and is said to be useful for many diseases, especially beneficial as a sedative and to treat disorders of the digestive and respiratory systems. In Pakistan it is included in several remedies for hemiplegia, Bell's palsy, and Parkinson's disease.
Nardostachys, which is native to the Himalayan foothills at high altitude, is used extensively in the Ayurvedic tradition. In fact, this herb may have been adopted into the Chinese tradition from India, with plants growing in the Western Chinese provinces of Yunnan and Sichuan (in the mountain regions) being the same species as the Indian variety. Nardostachys was recommended in the Ayurvedic tradition for nervous and spasmodic symptoms, such as heart palpitations, headache, shaking, and convulsions (4). The active constituents of nardostachys are similar to those found in valerian. In India, modern research with the herb has been aimed at examining new uses rather than the traditional ones: it is being examined for its liver protective effects, ability to increase nerve growth factor, and lipid lowering effects. In Germany and Japan, some interest in this herb as an alternative to valerian has been shown, in that preliminary experiments (in laboratory animals) show that it has an even lower toxicity than valerian (which already has low toxicity).
In China, Nardostachys chinensis (see Figure 3), as well as N. jatamansi, is widely used as an analgesic herb. Its Chinese name is gansong or gansongxiang (gan = dry; song refers to the location where it was originally collected, Songban in Sichuan Province; xiang = fragrant); presumably, the fresh herb was used in folk medicine, and it is the dried herb (gan) that is incorporated into the Materia Medica as an item on the herb markets. According to Oriental Materia Medica (3), it is traditionally used for treating pain in the chest and abdomen that results from qi stagnation associated with internal cold. The herb is warm and regulates qi, having a quality similar to some other fragrant herbs, such as cyperus (xiangfu), saussurea (muxiang), sandalwood (tanxiang), and aquilaria (chenxiang), which have similar applications in treating pain.
Patrinia is an herb that was not widely used in Chinese herbology (except as a folk remedy) until recently, when interest in its antibacterial action was stimulated by the search for effective compounds to fight infections. It has become particularly well-known for treating appendicitis (5), with adaptation of an ancient formula from the Jingüi Yaolue (ca. 220 A.D.) in which it is combined with aconite and coix. There is reference to an herb by the same name, baijiangcao, in the Shennong Bencao Jing (ca. 100 A.D.), but several unrelated herbs are now collected under this name, including Thlaspi arvensis (Cruciferae Family) and Sonchus barchyotus (Asteraceae Family); thus the identity of the original plant used is in doubt. The Chinese name refers to the smell of the root (bai = spoiled; jiang = a soy product; referring to the plant's smell like that of spoiled tofu; cao = weed). Traditionally, the herbs collected as baijiangcao have been used to remove toxic heat, resolve phlegm mass, vitalize blood, and resolve swellings. It is used for abscesses and other infectious conditions that are localized. According to the Bencao Gangmu, patrinia is good for discharging pus and removing blood stasis (6). The herb has been used as a folk remedy for postpartum abdominal pain due to blood stasis.
Two species of Patrinia are currently in common use in China: P. scabiosaefolia (see Figure 4) and P. villosa, though other species of this herb are also collected. According to Pharmacology and Applications of Chinese Materia Medica (7), the sedative action of patrinia is twice as strong as that of valerian. According to clinical trials, the herb is reported to successfully treat neurasthenia symptoms of dizziness, heaviness of the heat, palpitations, hypersensitivity to light and sound, emotional instability, and anorexia. It was also reported effective, usually in combination formulas, for treating infections with swelling, such as mumps, suppurative tonsillitis, appendicitis, and acute pancreatitis, as well as other infections without swellings. Pharmacology experiments reveal a weak antibacterial action (8), so the herb may function via immune system regulation rather than direct antiseptic action.
It is reported that side effects of patrinia are rarely seen (mainly dry mouth and gastric discomfort). The active ingredients are still under investigation, but include triterpene saponin glycosides (patrinosides), iridoids (as lactones), and volatile oils. As with nardostachys, research aimed at evaluating its ability to protect and regenerate liver cells is one of the areas of modern interest. Although the root of patrinia was traditionally the part used (as with valerian and nardostachys), now the whole plant of patrinia is collected for medicinal use, with the upper portion being the largest part.
Nardostachys was added to the Convention on International Trade in Endangered Species (CITES) in 1997 at the request of India. Only the bulk herb materials (whole and sliced roots) are currently restricted from trade; manufactured preparations, such as powders, pills, extracts, and teas are still permitted in trade. Neighboring Nepal also recognized the declining supplies of the herb, stating:
The new Constitution of the Kingdom of Nepal (1991) formally recognizes the need to preserve the environment and to use natural resources wisely. At present, six non-timber forest products- which are recognized as threatened with over-exploitation-are banned from export in unprocessed form: Jatamansi (Nardostachys grandiflora), Sugandhawal (Valeriana jatamansi), Sugandhakokila (Cinnamomum glaucescens), Sarpagandha (Rauwolfia serpentina), Jhyau (consisting of several species of lichens: Parmelia, Ramalina, Usnea, etc.), and the mineral Silajit (a natural form of asphalt). Concerning two other species, Panchaunle (Dactylorhiza hatagirea) and Yarsagumba (the fungus Cordyceps sinensis), even their collection is banned.
A similar situation exists with valerian. In the Balkans, a major source of the herb, valerian collection is now being limited. For example, the situation in Bulgaria has been summarized as follows:
Since 1991, wild-harvesting of, and trade in, threatened botanical drug species are subject to restrictions and prohibitions issued by the Ministry of the Environment. Several ordinances regulate the gathering, trade, and export of selected wild botanical drug species, with the aim of protecting them and their natural habitats, to re-establish wild populations, and to encourage cultivation of some species. These ordinances establish restrictions and prohibitions on collecting, trading, and exporting botanical drug species. At least 14 plant species are totally prohibited from being collected from the wild, traded and processed for commercial purposes. Thus, for example, the species marshmallow (Althaea officinalis), madder (Rubia tinctorium), valerian (Valeriana officinalis) must be cultivated for commercial use.
Cultivation of valerian and nardostachys has been rapidly developed in their natural regions of growth: valerian in Europe and nardostachys in the Himalayan region (including Pakistan, India, Nepal, and Bhutan).